"Generic minocin 50 mg amex, antibiotic mouthwash over the counter".
Y. Dan, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Clinical Director, Homer G. Phillips College of Osteopathic Medicine
The second major type of continence mechanism used in right colon pouches is the tapered and/or imbricated terminal ileum and ileocecal valve virus facts purchase 50 mg minocin amex. Here again the technique is rather simple infection blood pressure 50 mg minocin amex, with imbrication or plication of the ileocecal valve region along with tapering of the more proximal ileum in the fashion of a neourethra (Bejany and Politano antibiotics quinolones generic minocin 50 mg with visa, 1988; Lockhart, 1987; Rowland et al. One feature of right colon pouches that has been criticized is the loss of the ileocecal valve. Although this does result in an increased frequency of bowel movements for some patients in the short term, the majority will experience bowel regularity either through intestinal adaptation or with the use of pharmacologic therapy. However, some patients have developed rather striking diarrhea or steatorrhea after the loss of the ileocecal valve. This may be particularly true in pediatric patients in whom there is neurogenic bowel dysfunction. The third surgical principle in constructing the continence mechanism is the use of the intussuscepted nipple valve or the flap valve, which avoids the need for intussusception. The creation of nipple valves is by far the most technologically demanding of all the continence mechanisms, and it is associated with the highest complication and reoperation rates. There exists a significant learning curve before the surgeon achieves reproducible and dependable results. The appendix is rotated and implanted into the taenia; the cecal tube serves as the stoma. Furthermore, in the past three decades we have seen the introduction of numerous modifications of the original technique of Kock for construction of a stable nipple valve. The singular reason for all of these modifications is the rather disappointing long-term stability of the nipple valve in some patients. As a result, the group at the University of Southern California has developed the T pouch, which uses a flap valve (Stein et al. This procedure, which appears much simpler than the intussuscepted nipple valve, has been used to create a continence and an antireflux mechanism. Nipple valve failure from slippage or valve effacement can be anticipated in 10% to 15% of cases even in the hands of the very best and experienced surgeons. A final feature of stapled nipple valves is the potential for stone formation on exposed staples. This was greatly lessened by the omission of staples at the tip of the intussuscepted nipple valve, as suggested by Skinner et al. However, more proximal staples occasionally erode into the pouch and serve as a nidus for stone formation. These stones are usually manageable endoscopically with forceps extraction, or else with electrohydraulic or ultrasonic disintegration of the stone with subsequent forceps extraction of the staple. Although exposed staples may serve as a nidus for stone formation, continent urinary diversion results in more urinary excretion of calcium, magnesium, and phosphate as compared with ileal conduit diversion (Terai et al. Thus all patients undergoing continent diversion are at an increased risk for the formation of reservoir stones. The fourth major technique for constructing a continence mechanism is the provision of a hydraulic valve, as in the Benchekroun nipple (Benchekroun, 1987). In this procedure a small bowel segment is isolated, with subsequent reversed intussusception that effectively apposes the mucosal surfaces of the segment. Tacking sutures are placed on a portion of the circumference of the intussuscepted segment to stabilize the nipple valve while allowing urine to flow freely between the leaves of apposed ileal mucosa. As the pouch fills, hydraulic pressure closes the leaves, thereby ensuring continence. The premise of this technique is that as the reservoir fills, the pressure within the valve would also increase, resulting in continence. Concerns regarding stomal stenosis, especially in children, and nipple destabilization have resulted in this procedure being largely abandoned (Sanda et al. General Procedural Methodology During construction of the pouch, intraoperative testing for pouch integrity should always be performed. The continence mechanism is also tested for ease of catheterization as well as continence after the pouch construction has been completed.
Syndromes
- Name of product (as well as the ingredients and strength, if known)
- Convulsions (from swallowing substance)
- Loose or damaged teeth
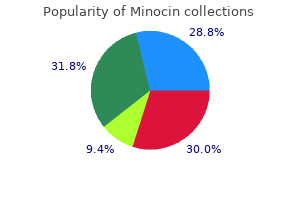
- Areas of interest may be quite narrow, such as an obsession with train schedules, phone books, a vacuum cleaner, or collections of objects.
- Anorexia nervosa
- Your symptoms get worse or do not improve with treatment
- Carpal tunnel biopsy
- Tumor of the hypothalamus (hypothalamic hamartoma)
- It is severe
To ensure restful sleep virus names list minocin 50 mg trusted, the smallercapacity pouches may be managed best with indwelling catheterization during sleeping hours latest antibiotics for acne minocin 50 mg cheap mastercard. Cutaneous Continent Urinary Diversion 3213 circumstances virus pictures minocin 50 mg purchase online, when the chimney of the nipple valve is not near the abdominal surface, the catheter may be misdirected into folds of bowel rather than into the nipple valve proper, resulting in urinary retention. Pouch urinary retention represents a true emergency, and the patient must seek immediate attention so that catheterization and drainage by experienced personnel can be achieved promptly. Rarely, use of a flexible cystoscope will be necessary with passage of a guide wire into the reservoir followed by a Council catheter. After the immediate problem has been resolved by emptying the pouch, a catheter should be left indwelling for 3 to 5 days to allow the edema and trauma to the catheterization portal to resolve. Before discharge, the patient should be observed to successfully self-catheterize on multiple occasions. Intraperitoneal rupture of catheterizable pouches has been reported (Kristiansen et al. In general, these episodes are more common in the neurologic patient in whom sensation of pouch fullness may be less distinct (Hensle, personal communication, 1993; Mitchell, personal communication, 1993). In general, these patients require immediate pouch decompression and radiographic pouch studies. For patients with large defects, surgical exploration and pouch repair are required. If the amount of urinary extravasation is small and the patient does not have evidence of peritonitis, catheter drainage and antibiotic administration may suffice in treating an intraperitoneal rupture. If there is any sign of progressive peritonitis, surgical exploration and repair are imperative. We have successfully employed this nonoperative approach on patients with ruptured right colon pouches. General Care Because all patients with catheterized pouches will have chronic bacteriuria, the problem of antibiotic management should be discussed. Most authors would suggest that bacteriuria in the absence of symptoms in patients with a urinary diversion does not warrant antibiotic treatment (Skinner et al. The construction of an effective antireflux mechanism in these pouches may help protect against clinical episodes of pyelonephritis, in contrast to patients with freely refluxing conduits. Obviously, if clinical pyelonephritis does occur, antibiotic treatment should be instituted. Episodes of recurrent pyelonephritis should be evaluated with radiography of the pouch to diagnose failure of the antireflux mechanism, upper tract stone formation, or ureteral stenosis. A condition termed "pouchitis" has been described that manifests with pain in the region of the pouch along with increased pouch contractility. This condition, although infrequent, may result in temporary failure of the continence mechanism because of the hypercontractility of the bowel segment employed for construction of the pouch. The patient typically has a history of sudden explosive discharge of urine through the continence mechanism (rather than dribbling incontinence), along with discomfort in the region of the pouch. It has been our experience that short courses of antibiotics are not usually successful in treating pouch infections. This may be because of the larger amount of foreign material in the form of mucus and sediment within intestinal pouches as opposed to the bladder. Therefore, whenever a pouch infection is diagnosed, antibiotic therapy should be continued for at least 10 days. Urinary retention is an infrequent but serious occurrence in catheterizable pouches. It is most commonly seen with pouches with continence mechanism consisting of a nipple valve. In these Continent Ileal Reservoir (Kock Pouch) this operation was first reported for use in urinary diversion by Kock et al. This report was singularly responsible for the renewed interest in continent diversion procedures at that time. An outgrowth of the Kock procedure for continent ileostomy (Kock, 1971), the Kock pouch combined reasonably dependable techniques for ensuring urinary continence and preventing reflux to the upper urinary tracts (nipple valves) with carefully refashioned bowel that provided a low-pressure urinary reservoir.
Syndromes
- Fever
- Use the cream twice a day for 7 to 10 days.
- Spasms of the hands or feet
- Lose weight if you are overweight.
- Dark brown urine
- If the medication was prescribed for the patient
- Bone density
- Various connective tissue and inflammatory diseases
- The amount swallowed
Multiple studies have linked obesity antibiotic brands minocin 50 mg buy discount online, diabetes infection blood buy 50 mg minocin, cardiovascular disease bacteria in urine culture buy 50 mg minocin, and neurologic disorders such as Parkinson disease and stroke to erectile dysfunction in elderly men (Garimella et al. Alterations in sex hormones and testis function have been shown to influence erectile function and cardiovascular health in elderly men (Rastrelli et al. Frailty affects multiple physical and psychosocial domains and has been shown to be linked to worse sexual health status (Lee et al. Other physical health issues may influence the ability to engage in sexual activity. Use of water-based lubricants and vaginal estrogen replacement therapy may be useful in these cases. Many chronic diseases that affect sexual health tend to be underreported and underdiagnosed among older adults. For example, hypogonadism, erectile dysfunction, and osteoporosis are conditions that influence sexuality and overall health that frequently remain undiagnosed in elderly men (Frost et al. Sexual health has also been closely linked to mental health in older adults, with higher rates of depression noted in those with erectile or sexual dysfunction (Cheng et al. Satisfactory sexual function has been linked to improved sense of well-being in older men and women (Lee et al. Chapter 128 Evaluation should be individually tailored to the clinical needs and goals of the patient and his or her caregivers. For example, improvement in volume or frequency of urinary leaking may allow someone who was previously confined to the home the ability to get out and interact in social settings more easily. The characteristics of incontinence, including duration, frequency and volume, should be determined. Any exacerbating factors such as physical activity, coughing, laughing, sneezing, or other factors should be assessed. This would include any prior treatments that have been attempted, and prior surgical records if available. Some patients will be unable to provide their own historical information, and portions of, or in some cases the entire, history may have to be obtained from caregivers or surrogates. For those older adults who reside in long-term care facilities, a call to the nursing staff member most familiar with them can help put clinical questions into better context. However, this is not always true, particularly for elderly patients who may have more complex voiding dysfunction. Similarly, urinary frequency is a common complaint that must be placed in clinical context. Voiding diaries can be helpful in gaining more insight into these clinical complaints. This can help to target treatments that can yield clinically meaningful improvements even if urinary leakage cannot be completely eliminated and is one of the main components of patient-centered therapy. In addition to routine aspects of physical examination including pelvic examination in women and genital and rectal examination in men, several unique components are also included for older adults with incontinence. The general physical examination should include identification of conditions associated with fluid overload and associated incontinence including peripheral edema, congestive heart failure, and pulmonary edema. Neurologic examination includes gait and balance, mobility, and ability to transfer between positions. This includes ability to get on and off a chair, which can be similar to getting on and off the toilet. Clinical signs associated with common rheumatologic and neurologic disorders in older adults should also be evaluated. These include changes from arthritis and joint disorders, Parkinson disease, multiple sclerosis, prior stroke, spinal stenosis, cord compression, vertebral disc herniation, acute or chronic back pain, dementia, and delirium. Perineal sensation should be tested and may be diminished or asymmetric, particularly in those with a history of underlying neurologic disease. For example, patients with a history of stroke and associated hemiparesis may have asymmetric perineal sensation.